Correlações neuroquímicas entre a depressão e as doenças neurodegenerativas

Recentemente foi aceito para publicação um artigo de revisão sobre a relação da depressão com doenças neurodegenerativas, tais como Alzheimer e Parkinson, bem como com o envelhecimento. Pacientes com doenças neurodegenerativas apresentam uma forte tendência em desenvolver também a depressão. As alterações cerebrais envolvidas nessas doenças são principalmente relacionadas com alterações nas funções e morfologia de células cerebrais. Mudanças hormonais, como o cortisol e em neurotransmissores, como a serotonina, também são um fator comum entre a depressão e as doenças neurodegenerativas. A neuroplasticidade, que é a capacidade que o cérebro tem de se adaptar e criar novas conexões está também alterada. A neuroinflamação e uma dimiuição na neurogênese foram demonstradas como fatores comuns entre a depressão, idade e doenças neurodegenerativas.
O estudo foi publicado por pesquisadores do laboratório de Neurociências da UNESC e The University of Texas Health Science Center at Houston.
Gislaine Z. Réus, Stephanie E. Titus, Helena M. Abelaira, Sharon M. Freitas, Talita Tuon, João Quevedo, Josiane Budni. Neurochemical correlation between major depressive disorder and neurodegenerative diseases. Life Science, 2016.
Mais informações: http://www.sciencedirect.com/science/article/pii/S0024320516303836
Por: Cenita Pereira 30 de junho de 2016 às 22:31Effect of folic acid on oxidative stress and behavioral changes in the animal model of schizophrenia induced by ketamine
Journal of Psychiatric Research, 2016, Pages 23–35
Alexandra I. Zugno, Lara Canever, Alexandra S. Heylmann, Patrícia G. Wessler, Amanda Steckert, Gustavo A. Mastella, Mariana B. de Oliveira, Louyse S. Damázio, Felipe D. Pacheco, Octacílio P. Calixto, Flávio P. Pereira,Tamires P. Macan, Thayara H. Pedro, Patrícia F. Schuck, João Quevedo, Josiane Budni.
Abstract: Recent studies have shown benefits for the supplementation of folic acid in schizophrenic patients. The aim of this study was to evaluate the effects of folic acid addition on adult rats, over a period of 7 or 14 days. It also sets out to verify any potential protective action using an animal model of schizophrenia induced by ketamine, in behavioral and biochemical parameters. This study used two protocols (acute and chronic) for the administration of ketamine at a dose of 25 mg/kg (i.p.). The folic acid was given by oral route in doses of 5, 10 and 50 mg/kg, once daily, for 7 and/or 14 days in order to compare the protective effects of folic acid. Thirty minutes after the last administration of ketamine, the locomotor and social interaction activities were evaluated, and immediately the brain structure were removed for biochemical analysis. In this study, ketamine was administered in a single dose or in doses over the course of 7 days increasing the animal’s locomotion. This study showed that the administration of folic acid over 7 days was unable to prevent hyper locomotion. In contrast, folic acid (10 and 50 mg/kg) administrated over a period of 14 days, was able to partially prevent the hyper locomotion. Our data indicates that both acute and chronic administrations of ketamine increased the time to first contact between the animals, while the increased latency for social contact was completely prevented by folic acid (5, 10 and 50 mg/kg). Chronic and acute administrations of ketamine also increased lipid peroxidation and protein carbonylation in brain. Folic acid (10 and 50 mg/kg) supplements showed protective effects on the oxidative damage found in the different brain structures evaluated. All together, the results indicate that nutritional supplementation with folic acid provides promising results in an animal model of schizophrenia induced by ketamine.
Mais informações: http://www.journalofpsychiatricresearch.com/article/S0022-3956(16)30120-0/abstract
Por: Cenita Pereira Borges 28 de junho de 2016 às 17:40QUADROS DE ANSIEDADE SÃO FREQUENTES NA POPULAÇÃO IDOSA DE CRICIÚMA
Estudo recente realizado pelo Laboratório de Neurociências da UNESC revelou que quadros de ansiedade são muito frequentes em idosos em comunidades da cidade de Criciúma. Ansiedade nos idosos se sobrepõem de forma significativa e estão associados a algumas variáveis clínicas cardiovasculares. O estudo foi publicado no Jornal Brasileiro de Psiquiatria.
Dados sobre a publicação:
MACHADO MB, IGNACIO ZM, JORNADA LK, RÉUS GZ, ABELAIRA HM, ARENT CO, SCHWALM MT, CERETTA RA, CERETTA LB, QUEVEDO J. Prevalência de transtornos ansiosos e algumas comorbidades em idosos: um estudo de base populacional. Jornal Brasileiro de Psiquiatria, v. 65, p. 28-35, 2016.
Por: Cenita Pereira Borges 26 de abril de 2016 às 10:03The amyloid hypothesis of Alzheimer's disease at 25 years.
EMBO Molecular Medicine. 2015, mar, 29.
Selkoe DJ, Hardy J.
Abstract:
Despite continuing debate about the amyloid β-protein (or Aβ hypothesis, new lines of evidence from laboratories and clinics worldwide support the concept that an imbalance between production and clearance of Aβ42 and related Aβ peptides is a very early, often initiating factor in Alzheimer'sdisease (AD). Confirmation that presenilin is the catalytic site of γ-secretase has provided a linchpin: all dominant mutations causing early-onsetADoccur either in the substrate (amyloid precursor protein,APP) or the protease (presenilin) of the reaction that generates Aβ. Duplication of the wild-typeAPPgene in Down's syndrome leads to Aβ deposits in the teens, followed by microgliosis, astrocytosis, and neurofibrillary tangles typical ofAD Apolipoprotein E4, which predisposes toADin > 40% of cases, has been found to impair Aβ clearance from the brain. Soluble oligomers of Aβ42 isolated fromADpatients' brains can decrease synapse number, inhibit long-term potentiation, and enhance long-term synaptic depression in rodent hippocampus, and injecting them into healthy rats impairs memory. The human oligomers also induce hyperphosphorylation of tau atAD-relevant epitopes and cause neuritic dystrophy in cultured neurons. Crossing humanAPPwith human tau transgenic mice enhances tau-positive neurotoxicity. In humans, new studies show that low cerebrospinal fluid (CSF) Aβ42 and amyloid-PETpositivity precede otherADmanifestations by many years. Most importantly, recent trials of three different Aβ antibodies (solanezumab, crenezumab, and aducanumab) have suggested a slowing of cognitive decline inpost hocanalyses of mildADsubjects. Although many factors contribute toADpathogenesis, Aβ dyshomeostasis has emerged as the most extensively validated and compelling therapeutic target.
Mais informações: http://www.ncbi.nlm.nih.gov/pubmed/27025652
Por: Cenita Pereira Borges 01 de abril de 2016 às 16:39Positive modulators of the a7 nicotinic receptor against neuroinflammation and cognitive impairment in Alzheimer’s disease
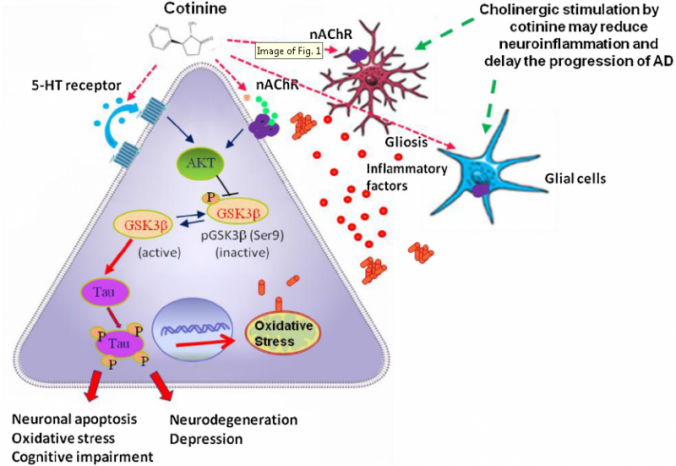
Revista: Progress in Neurobioligy. 2015, jan, 6.
Autores: Valentina Echeverria, Alex Yarkov, Gjumrakch Aliev.
Resumo:
Evidence so far indicates that therapies targeting a single aspect of Alzheimer’s disease (AD) have no sufficient efficacy in diminishing long-term the progression of AD. Neuroinflammation is an early event during the development of the disease and it is thought to exacerbate the abnormal aggregation of the amyloid beta peptide (Ab) and the microtubule associated protein Tau. Inhibition of gliosis is considered fundamental to reduce neuroinflammation, oxidative stress, apoptosis and synaptic dysfunction driving the progression of AD. Drugs that are able to target more than one aspect of the pathology may have higher chances of success. Modulators of a7 nicotinic acetylcholine receptors (a7nAChRs) such as nicotine and some of its derivatives have this potential because of their anti-inflammatory, antiapoptotic, pro-cognitive and anti-protein aggregation effects. However, the rapid desensitization of a7nAChRs is considered an important factor limiting its potential therapeutic use. In here, in light of current evidence, the objective of this review is to discuss the advantages and potential therapeutic value of positive allosteric modulators (PAMs) of the nAChRs in halting or delaying the progression of AD by diminishing neuroinflammation, abnormal protein aggregation and synaptic dysfunction.
Por: Cenita Pereira Borges 18 de março de 2016 às 18:53

 Newsletter
Newsletter  RSS
RSS